Laser Focal Therapy: What to Expect
A detailed outline of your patient journey
You will receive both email and phone contact information for our medical team so that you can always reach us. In addition, we conduct a pre-operative consultation prior to the procedure, we meet the day of the procedure, and will see you frequently in follow-up.
PRE-OPERATIVELY:
Our team will have collected and reviewed your medical records to evaluate you for inclusion and suitability. Our surgical team will have discussed your case during Tumor Board and conducted a surgical plan based on size, number, shape and location of ablation areas. Prior to the procedure, we will review the Informed Consent Document with you to ensure you understand every aspect of the procedure. We will discuss the risk, benefits, and paperwork of the procedure.
INTRA-OPERATIVELY:
The day of the procedure, our nurse will place an intravenous catheter (IV) in your arm so that she/he can administer IV antibiotics, pain medications and fluids (to maintain hydration). Should other medications be necessary, they will be administered through this IV as well.
You may have a urinary catheter placed so that we can provide cooled urethral saline through Continuous Bladder Irrigation (CBI) protection. This catheter remains in place depending on the size, shape, and location of treatment. Our urologist will perform the insertion and removal.
Patients are positioned on their stomach on the MRI table for the procedure. A small rectal probe (the diameter of an index finger in width) covered in numbing lidocaine jelly to allow access to the prostate. We use the transrectal route for laser fiber placement. This is minimally invasive (compared to thermocouples and transperineal needles), with fewer complications and less recurrence. Technical errors due to misregistration are also less frequent with transrectal fiber placement under MRI guidance.
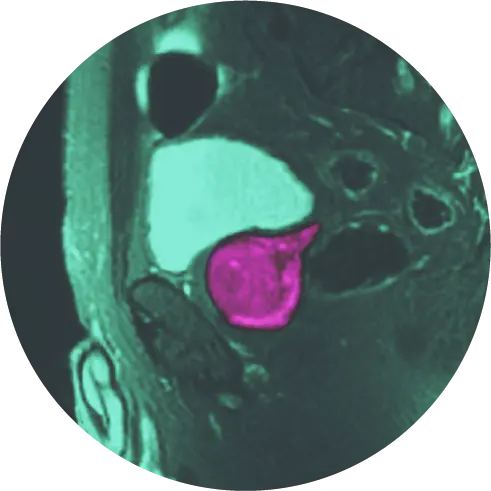
During the procedure, we will use real-time MRI to visualize the target, guide placement of the laser fiber, and ablate (destroy) cancer cells or for either cancer or BPH (an overgrown transitional zone) while protecting healthy tissue with “safety markers” that are positioned at the urethra and neurovascular bundle. This helps monitor sensitive structures to decrease risk of damage to urinary and sexual function.
POST-OPERATIVELY:
Patients will return home or to their hotel room after at least two hours in the recovery room that same day. They must be accompanied by a family member or care giver as driving is not permitted.
We see each patient again according to our rigorous follow-up protocol. This includes follow-up imaging, biopsy and PSA monitoring.
At HALO Dx we are mindful of the patient experience and acceptance of the technology. We do not offer endorectal coil for MRI for the same reasons, instead, we offer a high channel-count phased array pelvic coil. This surface coil is used for both diagnostic prostate imaging and allows access to biopsy and therapy.

Procedure Outline
- Pre-procedure MRI confirms the location and boundaries of the target(s).
- The DynaTRIM device is calibrated to the images, and the parameters (knobs) are adjusted to an appropriate three-dimensional approach.
- The thin, 1.85mm cooling cannula and FDA cleared laser fiber is then placed into the target through the inner channel of the rectal probe under MRI guidance. Continuous bladder irrigation (CBI) may be performed. The laser is then applied at low power “test dose” to confirm appropriate location with the heat from the laser being monitored with real time MRI thermometry in two separate planes. Only after this final confirmation, the team will increase the laser to treatment level power, monitor the tissue being ablated and make appropriate adjustments to contour the ablation zone.
- The laser fiber is usually then repositioned multiple times to provide overlapping ablations. Because we believe in obtaining wide margins, we will usually perform many overlapping ablations.
- At the end of the treatment, we evaluate the result with contrast enhanced MR imaging.