The American Cancer Society released new research that showed important but concerning trends in prostate cancer morbidity. This study shows that it’s more important than ever for men to follow their physician’s screening recommendations. After two decades of declining rates of prostate cancer diagnoses in the US, researchers observed annual increases in diagnoses between 2014 to 2019. The largest increase was seen in the number of men with advanced stage prostate cancer.1 Prostate cancer is considered advanced when the cancer spreads beyond the prostate gland to surrounding areas like the lymph nodes or the bones. This is also known as metastatic prostate cancer.
Treatments for advanced or metastatic cancer are more difficult and more aggressive with the potential to cause serious side effects that affect a person’s long-term quality of life. Prostate cancer affects 1 in 8 men and is the second leading cause of death for men in the US.2 The data presented in this report are worrisome sparking discussions about how to reverse this trend.
What Is Causing the Increase in Prostate Cancer Diagnoses?
One possible reason for the increase in advanced prostate cancer diagnoses could be the result of a push to reduce unnecessary prostate cancer screenings in the last fifteen years. Screenings help doctors catch prostate cancer at its earliest stages before it can progress to advanced disease. Between 2008 to 2018, the US Preventative Services Task Force (USPTF) adjusted their guidelines to advise against screenings for men under the age of 55 or over the age of 70.2
Prior to 2008, prostate cancer screening using the prostate-specific antigen (PSA) test was more widespread and accessible. The USPTF claimed that men at low risk of prostate cancer were undergoing screening that eventually led to overdiagnosis. Overdiagnosis refers to diagnosing cancer that is slow-growing and will likely never be harmful to a person. Overdiagnosis could lead to overtreatment where patients receive treatments that can have negative side-effects. To reduce overdiagnosis and overtreatment, the USPTF advised against routine PSA screening for many men.
Disparities in Prostate Cancer
The USPTF guidelines reducing PSA screenings didn’t account for men at higher risk for developing prostate cancer. In particular, Black men are much more likely to be diagnosed with prostate cancer compared to any other race. Death rates are also two to four times higher for Black men who develop prostate cancer.1 These disparities are well known and a huge cause for concern for the medical community. However, screening guidelines are not tailored to specific sub-groups of people. Many Black men who could have benefitted from screening before the age of 55 may have missed an opportunity to catch prostate cancer at an early stage.
The Importance of Early Detection and Screening
Prostate cancer is most treatable when it is diagnosed early. Early-stage prostate cancer has a survival rate of almost 100% compared to just 31% for those with advanced stage cancer.3 Early detection is key, and screening plays an important role.
The new data from the American Cancer Society may lead to a reevaluation of current screening guidelines to help ensure that doctors are catching prostate cancer before it advances to metastatic disease. Tailoring guidelines to subgroups of people like Black men or men with a family history of prostate cancer could help catch cancer in high-risk groups without subjecting low-risk individuals to extra testing and treatment. In the meantime, men in high-risk groups should have conversations with their doctors to discuss how screening might help them. Meeting with a specialist like a urologist can also help men receive expert guidance about prostate cancer.
Advances in Prostate Cancer Diagnostic Testing
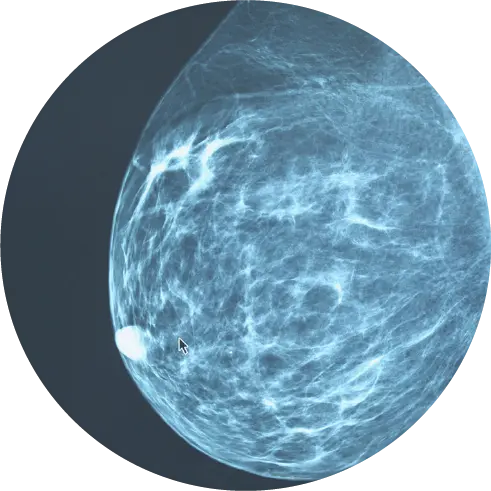
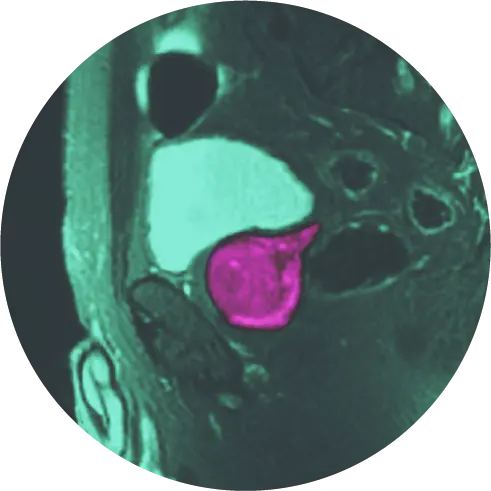
While the most common screening tool is the PSA test, recent scientific advances have led to additional tests to help detect prostate cancer. Precision diagnostics combines several tests to improve the detection rate and reduce the chance of missing significant disease. Diagnostic imaging like MRI, biomarker testing and genetics can be combined so the weakness of each test is reduced by the strengths of the other tests. Recent research has quantified the improvements. When the mpMRI, PSA density, and urine biomarkers are used together to select patients appropriate for biopsy, 99% of high-grade cancers are detected and 13.5% of unnecessary biopsies are safely avoided.4
Advances in Targeted Treatments
When prostate cancer is detected early, patients can benefit from treatments before the cancer has a chance to spread. Recent advances allow physicians to choose personalized treatments that have the best chance to address the patient’s prostate cancer type with the least amount of side-effects.
A personalized approach to treating prostate cancer also means a patient does not have to try numerous treatments to find one that works, preventing many of problems associated with overtreatment. Instead of trying invasive treatments like radiation or surgery, genomic testing can help determine if a non-invasive treatment options such as laser focal therapy or TULSA-Pro would help a patient.
Genomic testing allows doctors to look for certain signs called biomarkers that help them understand the potential growth of an individual’s specific tumor to identify which treatment options might work best for that person.5 Prostate cancer genomic testing can be done on the tissue from a positive prostate biopsy.
Moving Forward
Considering this update from the ACS, patients should begin or reopen the discussion about prostate cancer screening with their physicians. If recommended, patients should diligently follow their personalized screening guidelines. Detecting prostate cancer early enables patients to have more treatment options and dramatically increases chances of survival.
Precision diagnostics, where results of biomarker, imaging, and genetic testing are combined, will detect more significant cancers than isolated tests. These strategies can help patients survive cancer without long-term side effects that impact their quality of life.
With the HALO PathWay™, we combine advanced imaging, hereditary cancer testing, and urine biomarkers for earlier detection and to decrease unnecessary biopsies. For prostate cancer treatment, HALO’s laser focal therapy results in ≤1% ED and incontinence, as shown in clinical trial studies with 12-year follow up data. If you have received a high-PSA test result or a prostate cancer diagnosis, contact us to learn more about the HALO PathWay for prostate or laser focal therapy.
References
- https://pressroom.cancer.org/FactsandFigures23
- https://www.nbcnews.com/health/cancer/men-diagnosed-advanced-prostate-cancer-psa-testing-drops-rcna65277
- https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/survival-rates.html
- https://pubmed.ncbi.nlm.nih.gov/32897802/
- https://www.cancer.gov/about-cancer/treatment/types/biomarker-testing-cancer-treatment